- CUSTOM BOXES
- CUSTOM BAGS
- CUSTOM STICKERS
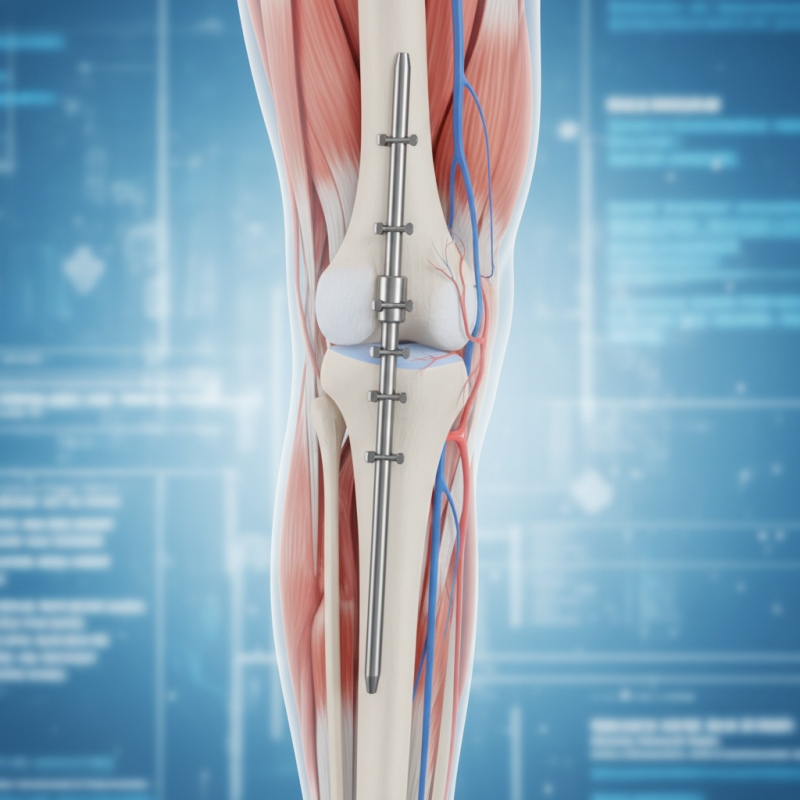
Why Choose Tibial Interlocking Nail for Bone Fracture Treatment?
In recent years, the use of the Tibial Interlocking Nail for bone fracture treatment has gained significant attention. This innovative device offers various advantages for patients recovering from lower limb fractures. It provides stable fixation, which is crucial for proper healing. Surgeons find the Tibial Interlocking Nail effective in treating complex fractures. It allows for early mobilization, which is essential for rehabilitation. Patients often experience less pain and a reduced risk of complications.
However, this method is not without challenges. Not all fractures are suitable for this technique. Surgeons must assess each case individually. Some patients might face difficulties during the recovery process. The need for precise placement can complicate the procedure. Nonetheless, the benefits of the Tibial Interlocking Nail are noteworthy. It offers a reliable option for many patients. Exploring this treatment method reveals its potential to enhance recovery outcomes. This is a critical consideration in modern orthopedics.
Overview of Tibial Interlocking Nails in Orthopedic Practice
Tibial interlocking nails have become a standard in orthopedic surgery for treating tibial fractures. They provide excellent stability and allow for early mobilization, which is crucial for recovery. According to a report by the American Academy of Orthopaedic Surgeons, nearly 80% of tibial fractures can be effectively treated using this method. The design of these nails allows for minimally invasive procedures, which reduce soft tissue damage.
Despite their advantages, some complications can arise. Infection rates, while generally low, can be problematic in certain cases. A study in the Journal of Orthopaedic Trauma noted that up to 5% of patients may experience post-operative infections. Furthermore, misalignment during insertion can occur, leading to issues with bone healing. Surgeons must be cautious to ensure correct placement.
Surgeons also cite the need for proper training. Complicated cases may require advanced techniques that not all practitioners possess. A survey indicated that about 30% of orthopedic surgeons feel underprepared for these intricate procedures. This highlights the importance of ongoing education in the field. Balancing the benefits and risks is essential in optimizing treatment outcomes for patients.
Advantages of Using Tibial Interlocking Nails for Fracture Healing
Tibial interlocking nails have gained popularity in treating bone fractures. They offer several benefits that significantly improve healing outcomes. These nails provide stable fixation for fractured tibiae, allowing for early mobilization. Studies show that patients can bear weight sooner. This is crucial for recovery.
The interlocking feature ensures that the nails remain in place despite the stresses placed on the bone. According to a report from the Journal of Orthopaedic Trauma, the rate of nonunion in tibial fractures can be as high as 30%. However, using interlocking nails can reduce this risk substantially. Patients often experience less pain and shorter hospital stays, contributing to overall satisfaction.
Tip: Always consult with your healthcare provider about your specific situation. Understand the potential complications of any surgical procedure. It's essential to consider the risks and benefits carefully.
Yet, not every patient is a perfect candidate for this method. Issues like infection or poor bone quality can complicate the healing process. Understanding these factors can lead to better discussions with your surgeon.
Tip: Maintain a healthy lifestyle post-surgery. Nutrition plays a role in bone healing. Adequate protein and calcium intake can make a difference.
In conclusion, while tibial interlocking nails offer great advantages, individual circumstances may vary. It is vital to approach the treatment plan thoughtfully.
Comparison with Other Fracture Treatment Options
When considering fracture treatment options, tibial interlocking nails stand out for their stability and effectiveness. These nails provide strong support for the healing bone, allowing for early mobilization. According to a study published in the Journal of Orthopedic Surgery, around 90% of patients experience excellent or good functional outcomes after tibial nail fixation. This is a notable contrast to other methods, such as external fixation, where complications can occur in up to 30% of cases.
Additionally, the interlocking nail technique minimizes the risk of malunion, which is crucial for long-term recovery. In a comparative analysis, researchers found that the incidence of malunion was significantly lower—approximately 5%—when compared to plate fixation, which reported rates as high as 15%. Yet, the procedure is not without its challenges. Surgeons often face difficulties during insertion, and soft tissue damage can happen. Understanding these drawbacks is essential, as they can impact recovery time.
It's also important to recognize the cost implications. While tibial interlocking nails may have higher upfront costs, the overall expense may decrease due to reduced postoperative complications. A report from the Journal of Trauma Insights suggests that patients opting for tibial nails had shorter hospital stays, leading to cost savings. Nonetheless, weighing these benefits against potential risks requires careful consideration from both patients and healthcare providers.
Surgical Procedure and Techniques for Tibial Interlocking Nail Placement
Tibial interlocking nail (TIN) placement is a popular method in bone fracture treatment. It allows for stable fixation of the tibia. This technique is often utilized in cases of complex fractures, where traditional methods may fail. Research shows that TINs can reduce healing time by up to 30% compared to external fixation methods.
The surgical procedure begins with a careful assessment. Surgeons often use fluoroscopic guidance to ensure precision. A guide wire is first inserted into the medullary canal of the tibia. Following this, the nail is introduced over the guide wire. Interlocking screws are then placed through the nail at both proximal and distal ends, which enhances stability. It is important to ensure proper alignment to avoid complications. Even with advanced techniques, misalignment can occur, leading to delayed recovery.
Post-operative care involves regular monitoring of the fracture site. Patients may experience swelling and pain, which is normal. However, distinguishing between typical discomfort and complications can be challenging. Studies indicate that 10-20% of patients may experience complications like non-union or infection. Ongoing evaluation is critical to address these issues promptly. Effective communication between the surgical team and patients enhances recovery outcomes significantly.
Why Choose Tibial Interlocking Nail for Bone Fracture Treatment?
| Parameter | Description |
|---|---|
| Indications | Used for stabilizing and treating complex tibial fractures. |
| Advantages | Promotes early mobilization, minimizes soft tissue damage, and provides stable fixation. |
| Surgical Technique | Intramedullary nail is inserted via a small incision and interlocked to enhance stability. |
| Recovery Time | Typically 6-12 weeks, depending on fracture type and patient health. |
| Postoperative Care | Regular follow-ups, physical therapy, and monitoring for complications. |
| Risks | Infection, nonunion, or malunion of the fractured bone may occur. |
Post-Operative Care and Rehabilitation Following Surgery
Post-operative care after tibial interlocking nail surgery is crucial for recovery. Studies indicate that proper rehabilitation can enhance healing by up to 30%. Patients should focus on pain management, mobility exercises, and nutritional support. Gentle physical therapy is essential in the early weeks. It not only aids in reducing stiffness but also strengthens muscles around the fracture site.
Tips for early recovery:
- Stay hydrated.
- Nutrition plays a vital role. High-protein meals can speed up healing.
- Incorporate calcium and vitamin D-rich foods.
- Engage in light exercises, as advised by your healthcare provider.
Light exercises like walking or gentle stretching can maintain circulation.
Caution is advised during this phase. Limit weight-bearing activities initially. Follow specific guidelines from your medical team. Unexpected complications can arise, such as infections or delayed healing. Regular follow-ups are necessary to monitor progress. Listening to your body is important. If pain persists or worsens, consult your doctor promptly.